Last Updated on April 4, 2020
CBC or Complete blood count is a series of tests cried out on a blood sample that give information about the cells circulating within the blood.
There are three main types of cells which circulate in the bloodstream
- Red blood cells (RBCs or erythrocytes)
- White blood cells (WBCs or leukocytes)
- Platelets (thrombocytes).
RBCs provide oxygen to all the cells in the body, WBCs help fight infection in the body, and platelets help stop bleeding after an injury.
Information about these cells can provide important clues about the overall health of the body. Any abnormality in these cells, whether related to their number (abnormally high or low counts) or related to their morphology (i.e., structure) may indicate some underlying disease.
CBC thus gives very useful information about these blood cells which help in the identification of a number of hematological (blood-related) disorders.
CBC is a very common, routinely performed first-line investigation for any suspected disorder.
It is also performed as a routine health check-up
Cell Types in Blood
A summary of various cells present in the blood, their percentage and significance of changes is mentioned below
DLC |
%age |
Absolute count ( x 10 9/L) |
Normal function in body |
Increase in count |
Decrease in count |
| Neutrophils | 40-75 % | 2.0 – 7.5 | Also called polymorphonuclear leucocytes. These cells protect the body from bacterial and fungal infections. They are first line of defense against microbial infections. | Neutrophilia
– Acute bacterial infections -Acute inflammatory conditions- acute appendicitis – Leukemia
|
Neutropenia
– Severe overwhelming infection – Infections like typhoid, influenza, rocky mountain spotted fever – Aplastic anemia – Bone marrow damage (e.g., chemotherapy, radiation therapy – Leukemia |
| Lymphocytes | 20-40 % | 1.5 – 4.0 | These cells protect the body against viruses, bacteria, and fungi. They can either directly attack these microbes or produce antibodies that attack and destroy them. | Lymphocytosis
-Chronic infections -Viral diseases – Aplastic anemia -Leukemias – Lymphomas Normal physiological lymphocytosis is seen in children less than 8 years of age. |
Lymphocytopenia
-Infections like HIV, viral hepatitis -Autoimmune disorders, -Bone marrow damage in case of chemotherapy, radiation therapy -Corticosteroids
|
| Monocytes | 2-8 % | 0.2 – 0.8 | They have a phagocytic function (consume dead or damaged cells) like neutrophils. They however live longer than neutrophils. They eventually leave the bloodstream and become tissue macrophages, which remove dead cell debris as well as attack microorganisms. | Monocytosis
-Infections like malaria, Kala-azar, tuberculosis -Certain leukemias |
Not of much significance |
| Eosinophils | 1-6 % | 0.04 -0.4 | They have a role in allergic reactions and parasitic infections. They secrete chemicals that destroy parasites | Eosinophilia
-Allergic conditions / asthma -Parasitic infestations -Hypereosinophilic syndrome -Some cancers, Hodgkin’s lymphoma, leukemias |
Not of much significance |
| Basophils | <1 % | 0.01 -0.1 | These cells release histamines during allergic reactions | Basophilia
– Chronic myeloid leukemia – Myelofibrosis – Urticaria pigmentosa |
Not of much significance |
How is Complete Blood Count Done?
It is performed by drawing a few milliliters of blood from a vein. Most commonly, the sample is obtained from a vein that is visible from the skin, such as a vein on the inner angle of the elbow (antecubital fossa) or the back of the hand.
No prior preparation or fasting is required.
It can be performed manually or by using automated techniques.
Manual method for Complete Blood Count
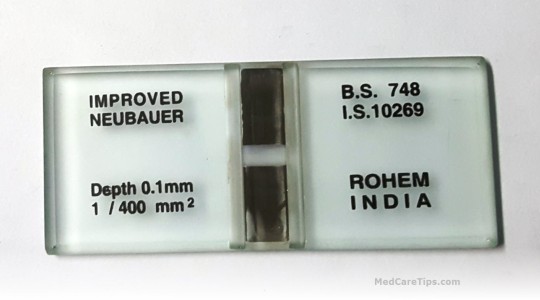
A counting chamber or hemocytometer is used to calculate various parameters. It is carried out in low resourced settings or labs. It can give erroneous results because of human error as well as sampling error as very few cells are counted in comparison with automated techniques. It is, however, useful in cases where abnormal cells are present in the blood and automatic analyzers cannot identify them accurately.
Automated methods for Complete Blood Count
Automated methods include measurement of blood parameters in CBC by automated counters. Automated methods have increased accuracy and speed and are being increasingly preferred over manual methods. The automated counters may not be able to identify and categorize few abnormal cells, in which case the results need to be reviewed manually.

Two major types are available
- That depend on changes in impedance in electric flow
- That use differences in light scatter properties. The instrument identifies blood cells by analyzing data about their size and aspects of light as they pass through the cells (called front and side scatter).
What does a Complete Blood Count Report ?
The various parameters included in a CBC report include:
Hemoglobin (Hb)
This is the amount of hemoglobin in a volume of blood. Hemoglobin is the protein molecule within RBCs that carries oxygen and gives blood its red color.
Hematocrit (Hct) or Packed cell Volume (PCV)
It is the ratio of the volume of red cells to the volume of whole blood. It signifies the amount of space in blood that is occupied by RBCs. Its value is affected by the number of RBCs and by the size of the RBCs.
Red blood cell count (RBC count or erythrocyte count)
It signifies the actual number of red blood cells in a volume of blood.
Red blood cell indices
Red cell indices are calculations that provide information on the physical characteristics of the red blood cells. These include
Mean corpuscular volume (MCV)
It is a measurement of the average volume of a single red blood cell. Small-sized RBCs result in a lower MCV, while larger RBCs result in a higher MCV. It is calculated as dividing Hematocrit by RBC and multiplying by 10.
(Hct÷ RBC) x 10
Mean corpuscular hemoglobin (MCH)
It is the average amount of hemoglobin inside a single red blood cell. RBCs with more hemoglobin result in a higher MCH and vice versa. It is calculated as
(Hb÷ RBC) x 10
Mean corpuscular hemoglobin concentration (MCHC)
It is the average concentration of hemoglobin inside a single red blood cell. It is calculated as
(Hb x 100)÷Hct
Red blood cell distribution width (RDW)
It signifies the variation in the size of RBCs. All RBCs are not of the same size. The RDW measurement is affected by the size of the smallest RBC and the size of the largest RBC.
White blood cell count or Total leucocyte count (WBC or TLC)
It is the total number of leucocytes in a volume of blood.
White blood cell differential count or Differential leucocyte count (DLC)
It measures the different white cell types as a percentage and as an absolute number per liter. The different types of leucocytes are neutrophils, lynphocytes, monocytes, eosinophils and basophils.
Platelet (thrombocyte) Count
It gives the total number of platelets in a specified volume of blood.
Mean platelet volume (MPV)
It measures the average size of platelets in a volume of blood.
Interpretation of Complete Blood Count Report
A sample report of CBC is given below
| Parameter | Normal range | unit |
| Hb | Men:13-17
Women:12-16 |
g/dl |
| Hct/ PCV | Men: 40-50
Women:35-45 |
% |
| RBC | Men: 4.5-5.5
Women:3.5-4.5 |
X 10 12/L |
| MCV | 80.0-100.0 | fl |
| MCH | 27.0-32.0 | pg |
| MCHC | 32.0-35.0 | g/dl |
| RDW | 11.5-14.5 (as coefficient of variation)
39.0-45.0 (as standard deviation) |
%
fl |
| WBC/ TLC | 4.0-11.0 | X 10 9/L |
| Platelet count | 150.0-400.0 | X 10 9/L |
| MPV | 7.5-11.5 | fL |
Hemoglobin, RBC count and hematocrit
The results of these tests are related because they measure aspects of RBCs.
If the values are lower than normal, the patient has anemia. Anemia has many causes. The most common ones include low levels of iron, vitamin B 12 or folic acid, blood loss, some underlying inherited condition like thalassemia, leukemia, etc.
If RBC count is higher than normal (erythrocytosis), or patient has high hemoglobin or hematocrit levels, there could be an underlying condition, such as polycythemia vera or heart disease.
Red Cell Indices
To find out the exact cause of anemia, red blood cell indices (MCV, MCH, MCHC) and RDW are useful. The indices will show lower value in case of microcytic hypochromic anemias (most common cause of which is iron deficiency).
Higher than normal value of indices is observed in macrocytic anemias (most common cause of which is vitamin B 12 or folic acid deficiency).
Anemia in the presence of normal indices is indicative of normocytic normochromic anemias (commonly seen in case of blood loss) or dimorphic anemias (when dual population of microcytic hypochromic and macrocytic cells are present). Additional testing may be required to determine the exact cause of anemia.
White Blood Cell Count
A low WBC count (leukopenia) is seen in severe overwhelming bacterial infection, autoimmune disorder that destroys white blood cells, bone marrow disorders or leukemias. Certain medications like chemotherapy can also cause white blood cell counts to drop.
A high WBC count (leukocytosis) is seen in infections, inflammation, immune system disorder or a bone marrow disease including leukemias. A high count can also be because of a reaction to medication.
A machine-generated percentage of the different types of white blood cells is called the automated WBC differential. These components can also be counted under the microscope on a glass slide by a trained laboratory technician or a doctor and referred to as the manual WBC differential.
Platelet count
A low platelet count (thrombocytopenia) can occur in certain infections like dengue fever, aplastic anemia, megaloblastic anemia, hypersplenism, idiopathic thrombocytopenic purpura or leukemias.
A high platelet count (thrombocytosis) is seen in iron deficiency anemia, post-hemorrhage, idiopathic thrombocythemia or chronic myeloid leukemia.
Role of Peripheral Blood Smear as Adjunct to Complete Blood Count
A peripheral blood film or smear examination (PBF or PS) can be done at the same time as a complete blood count. This test however is not part of regular complete blood count. A drop of blood is spread on a glass slide and stained with a special dye. The slide thus prepared is examined under a microscope.
The number, size, and shape of different blood cells is noted along with the presence of any abnormal cells. The appearance of RBCs helps to differentiate between various types of anemia. Certain cell types like blasts, promyelocytes, myelocytes, metamyelocytes, nucleated RBCs, etc are not normally seen in blood. Presence of any of these cells in the blood smear indicates follow-up or further investigations. Presence of hemo-parasites like malaria, filaria, etc is also looked for and species identification is carried out.
Read more about Peripheral Blood Smear: Procedure and Interpretation
