Last Updated on April 19, 2020
The skin is an important organ covers the entire external surface of the human body and it serves as a protective barrier that prevents internal tissues.
Skin is a dynamic organ that undergoes continuous changes throughout life as outer layers are shed and replaced by inner layers. Skin also varies in thickness among anatomic location, sex, and age of the individual.
Skin is thickest on the palms and soles of the feet (1.5 mm thick), while the thinnest skin is found on the eyelids and in the postauricular region (0.05 mm thick).
Layers of Skin
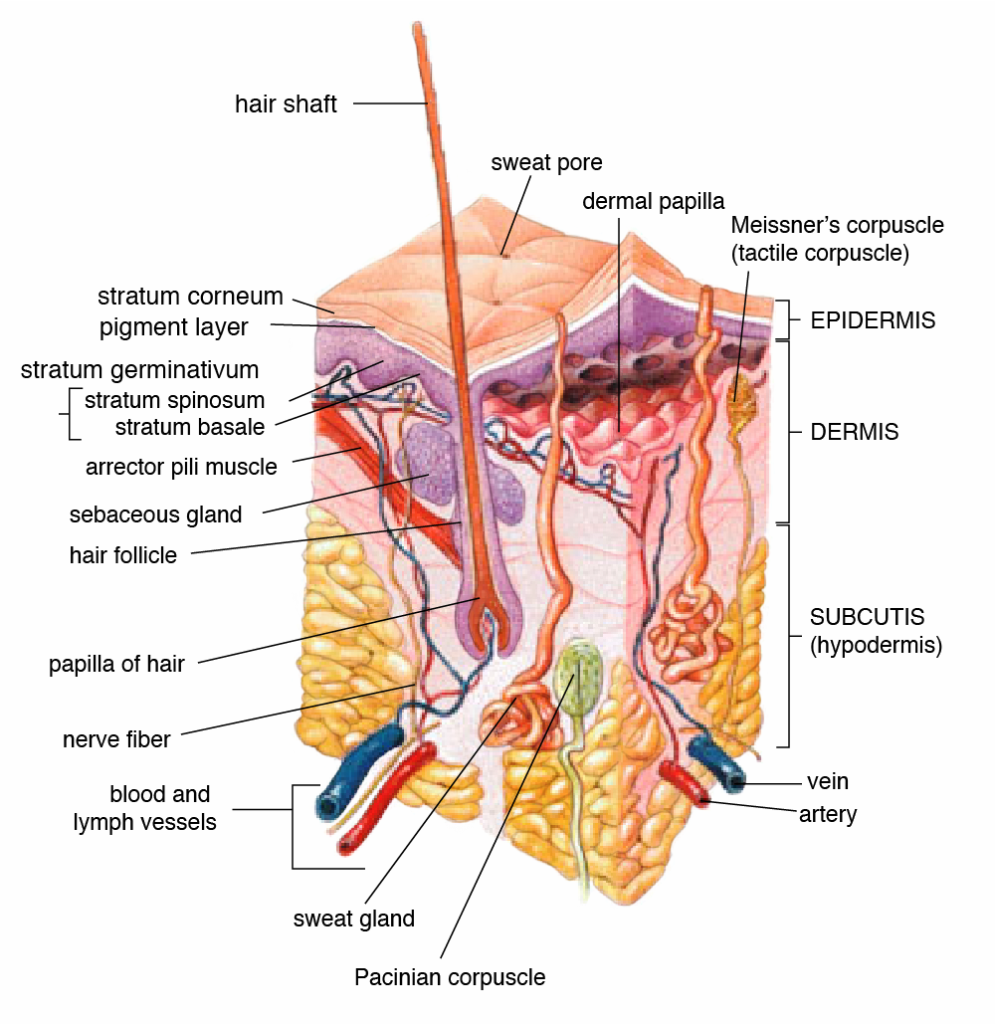
The skin has three layers-
- The epidermis is the outermost layer of skin. It provides a waterproof barrier and creates our skin tone.
- The dermis is below the epidermis. It contains tough connective tissue, hair follicles, and sweat glands.
- The deeper subcutaneous tissue (hypodermis) is made of fat and connective tissue.
The epidermis is derived primarily from surface ectoderm but contains melanocytes of neural crest origin, antigen-processing Langerhans cells of bone marrow origin, and pressure-sensing Merkel cells of neural crest origin.
The dermis is derived primarily from mesoderm and contains collagen, elastic fibers, blood vessels, sensory structures, and fibroblasts.
Epidermis
The epidermis is a stratified, squamous epithelium that consists primarily of keratinocytes. Keratinocytes are in progressive stages of differentiation from deeper to more superficial layers.
The epidermis has no blood vessels within it and is entirely dependent on the underlying dermis for nutrition and waste disposal via diffusion through the dermo-epidermal junction.
It is made of four or five layers of epithelial cells, depending on its location in the body.
Most of the skin can be classified as thin skin that has four layers – the stratum basale, stratum spinosum, stratum granulosum, and stratum corneum.
Thick skin is found only on the palms of the hands and the soles of the feet and has a fifth layer, called the stratum lucidum, located between the stratum corneum and the stratum granulosum.
The cells in all of the layers except the stratum basale are called keratinocytes.
Stratum Basale
The stratum basale is also called the stratum germinativum and is the deepest epidermal layer. It attaches the epidermis to the basal lamina, below which lie the layers of the dermis.
The cells in the stratum basale bind to the dermis via intertwining collagen fibers referred to as the basement membrane.
Dermal papillae are finger-like projections or folds in the superficial portion of the dermis. Dermal papillae increase the strength of the connection between the epidermis and dermis.
The stratum basale is a single layer of cells primarily made of basal cells. Keratinocytes are produced from this layer of cells, which are constantly going through mitosis to produce new cells. As new cells are formed, the existing cells are pushed superficially away from the stratum basale.
Merkel cells [a neural receptor especially abundant in the hands and feet] and melanocytes [cells that produce the pigment melanin and give hair and skin their color] are found dispersed among the basal cells in the stratum basale.
Stratum Spinosum
The stratum spinosum is spiny in appearance due to the protruding cell processes that join the cells via a structure called a desmosome.
The stratum spinosum is composed of 8-10 layers of keratinocytes. Langerhans cell, a type of dendritic cell is interspersed in this layer. It functions as a macrophage by engulfing bacteria, foreign particles, and damaged cells that occur in this layer.
The keratinocytes in the stratum spinosum begin the synthesis of keratin and release a water-repelling glycolipid. These help prevent water loss from the body and make the skin relatively waterproof.
With the production of new keratinocytes from stratum basale, keratinocytes of the stratum spinosum are pushed into the stratum granulosum.
Stratum Granulosum
The stratum granulosum has a grainy appearance. This occurs due to changes in the keratinocytes as they are pushed from the stratum spinosum. These changes are
- Cells become flatter
- Their cell membranes thicken
- They generate large amounts of the proteins keratin and keratohyalin [accumulate as lamellar granules within the cells which give the layer its grainy appearance]
The cells are 3-5 layers deep. The nuclei and other cell organelles disintegrate as the cells die and the keratin, keratohyalin, and cell membranes form the stratum lucidum, the stratum corneum, and the accessory structures of hair and nails.
Stratum Lucidum
The stratum lucidum is just above the stratum granulosum and below the stratum corneum. This smooth, seemingly translucent layer of cells is found only in the thick skin of the palms, soles, and digits and consists of dead and flattened cells. The transparency is imparted by eleidin, a clear protein rich in lipids, derived from keratohyalin. It also provides a barrier to water.
Stratum Corneum
The stratum corneum is the most superficial layer of the epidermis. The increased keratinization or cornification of the cells in this layer gives it its name. There are usually 15 to 30 layers of cells in the stratum corneum.
It is a dry, dead layer. Cells in this layer are shed periodically and are replaced by cells pushed up from the stratum granulosum (or stratum lucidum in the case of the palms and soles of feet). The entire layer is replaced during a period of about 4 weeks.
Cells in Epidermis
Keratinocytes
The cells in all of the layers except the stratum basale are called keratinocytes. Keratinocyte manufacture and store the protein keratin which gives hair, nails, and skin their hardness and water-resistant properties.
Keratinocytes are produced in the stratum germinativum, or the basal layer which is immediately superficial to the dermo-epidermal junction.
As keratinocytes divide and differentiate, they move from this deeper layer to the more superficial layers. Once they reach the stratum corneum, they are fully differentiated keratinocytes devoid of nuclei and are subsequently shed in the process of epidermal turnover.
Melanocytes
Melanocytes are derived from neural crest cells and function to produce a pigment, melanin which accumulates in organelles termed melanosomes.
Ultimately, the melanosomes are transferred via phagocytosis to the adjacent keratinocytes where they remain as granules. Melanocytes are found in the basal layer of the epidermis as well as in hair follicles, the retina, uveal tract, and leptomeninges.
Sun exposure, melanocyte-stimulating hormone (MSH), adrenocorticotropic hormone (ACTH), estrogens, and progesterone stimulate melanin production. Melanocytes have no ability to reproduce.
Langerhans cells
Langerhans cells originate from the bone marrow and are found in the basal, spinous, and granular layers of the epidermis. They serve as antigen-presenting cells.
Merkel cells
Merkel cells are touch receptors derived from neural crest cells, are found on the volar aspect of digits, in nail beds, on the genitalia, and in other areas of the skin.
Epidermal Appendages
Epidermal appendages or skin adnexa are intradermal epithelial structures lined with epithelial cells with the potential for division and differentiation. After the injury, all adnexal structures are capable of reepithelialization via the migration of keratinocytes from adnexal epithelium to the surface of the epidermis.
Epidermal appendages include the following
Eccrine Sweat Glands
Eccrine sweat glands are involved in the regulation of heat and are most abundant on the soles of the feet and least plentiful on the back. These originate as a band of epithelial cells growing downward from the epidermal ridge. They have three composite parts of the eccrine sweat unit, which are the intraepidermal spiral duct, the straight dermal portion, and the secretory coil.
The spiral duct opens onto the skin surface.
Apocrine Sweat Glands
Apocrine glands are involved in scent release and are confined mainly to the regions of the axillae and perineum. The intraepithelial duct opens into pilosebaceous follicles.
Apocrine sweat glands develop their secretory portions and become active just before puberty.
Apoeccrine Sweat Glands
The apoeccrine sweat glands develop during puberty from eccrine-like precursors, opening directly onto the skin. These are found in the adult axillae.
Hair follicles
Hair follicles vary considerably in size and shape, depending on their location, but they all have the same basic structure. The number and distribution of hair follicles over the body and the future phenotype of each hair are established during fetal development.
The sebaceous gland forms from a bud in the fetal hair follicle.
The arrector pili are a smooth muscle bundle that attaches to the external root sheath of the follicle.
Matrix cells in the hair bulb are responsible for the production of the hair shaft as well as the inner and outer root sheaths.
Hair color is determined by the distribution of melanosomes in the hair shaft.
Sebaceous Glands
Sebaceous glands are found in greatest number on the face and scalp but are present nearly everywhere with the exception of the tarsal plate of the eyelids, the buccal mucosa and vermilion borders of the lip, the prepuce and mucosa lateral to the penile frenulum, the labia minora, and the female areola.
Cells of the sebaceous glands contain abundant lipid droplets known as sebum in their cytoplasm and are arranged into lobules in the upper segment of the hair follicle.
The sebaceous glands are thought to be evolutionarily important in providing a secondary lubrication during the passage through the birth canal.
Nails
Fingernails provide protection to the fingertips, enhance sensation, and allow small objects to be grasped. The underlying nail bed is part of the nail matrix containing blood vessels, nerves, and melanocytes and has parallel rete ridges. The nail plate is formed from matrix keratinocytes.
Fingernails grow at an average rate of 0.1 mm per day, two to three times faster than the rate of toenail growth.
Dermo-epidermal Junction
The dermo-epidermal junction is an undulating basement membrane that adheres the epidermis to the dermis. It is composed of 2 layers, the lamina lucida and lamina densa.
The lamina lucida is thinner and lies directly beneath the basal layer of epidermal keratinocytes. The thicker lamina densa is in direct contact with the underlying dermis.
Dermis
The dermis is the layer that supports and sustains the epidermis.
The dermis is made of two layers of connective tissue
- Papillary Layer
- Reticular Layer
Papillary Layer
The papillary layer is made of loose, areolar connective tissue [collagen and elastin fibers]. This superficial layer of the dermis projects into the stratum basale of the epidermis to form finger-like dermal papillae.
The papillary layer contains fibroblasts, a small number of fat cells and small blood vessels.
This layer also contains phagocytes, lymphatic capillaries, nerve fibers, and touch receptors called the Meissner corpuscles.
Reticular Layer
This layer is thicker and composed of dense, irregular connective tissue. It is well-vascularized rich in sensory and sympathetic nerve supply. The reticular layer appears reticulated (net-like) due to a tight meshwork of fibers.
The fibroblast is the major cell type of the dermis. These cells produce and secrete procollagen and elastic fibers.
Elastin fibers provide some elasticity and collagen fibers provide structural and tensile strength, with strands of collagen extending into both the papillary layer and the hypodermis.
Collagen binds water to keep the skin hydrated. The reticular layer also contains fibroblasts, mast cells, nerve endings, lymphatics, and epidermal appendages. Surrounding the components of the dermis is the gel-like ground substance, composed of mucopolysaccharides (primarily hyaluronic acid), chondroitin sulfates, and glycoproteins.
The deep surface of the dermis is highly irregular and borders the subcutaneous layer, the panniculus adiposus, which additionally cushions the skin.
Hypodermis
The hypodermis or the subcutaneous layer or superficial fascia is a layer directly below the dermis. It connects the skin to the underlying fascia (fibrous tissue) of the bones and muscles.
It is not strictly a part of the skin, although the border between the hypodermis and dermis can be difficult to distinguish. The hypodermis consists of well-vascularized, loose, areolar connective tissue and adipose tissue, that provide for fat storage and provides insulation and cushioning for the integument.
Blood Supply of Skin
The cutaneous vessels originate either directly from the septocutaneous or fasciocutaneous perforators or as terminal branches of muscular vessels (musculocutaneous perforators).
In the skin, the vessels travel within or adjacent to the connective tissue framework and supply branches to each tissue with which they come into close contact (bone, muscle, fascia, nerve, fat). They also form extensive subdermal and dermal plexuses. The dermal vasculature is made up of two intercommunicating plexuses: the subpapillary or superficial plexus and the lower plexus at the dermal-subcutaneous interface.
The vessels anastomose extensively with other cutaneous vessels to form a continuous vascular network within the skin.
Muscles in Skin
Involuntary or smooth muscle of the skin occurs as arrector pili, tunica dartos of the external genitals, and the areolas around the nipples.
The muscle fibers of the arrector pilorum are located in the connective tissue of the upper dermis and are attached to the hair follicle below the sebaceous glands. When contracted, the hair follicle is pulled into a vertical position, deforming the skin and causing gooseflesh.
Striated or voluntary muscle is found in the skin of the neck as platysma and in the skin of the face as the muscle of expression.
Lymphatics
Blind-ended lymphatic capillaries arise within the interstitial spaces of the dermal papillae. These unvalved, superficial dermal vessels drain into valved deep dermal and subdermal plexuses.
These coalesce to form larger lymphatic channels, which course through numerous lymph nodes on their way to join the venous circulation near the subclavian vein – internal jugular vein junction bilaterally.
Read more about Lymphatic System-Structure and Function
Read more about Lymph Node-Structure and Function
Skin Innervation
The skin has specialized structures to detect various stimuli.
These include
- Merkel cells of the epidermis which detect light touch.
- Meissner corpuscles also detect light touch. These are found in the dermal papillae and are most concentrated in the fingertips.
- Pacini corpuscles are found deep within the dermis or even in the subcutaneous tissue. These structures are specialized to detect pressure.
- Krause bulbs detect cold
- Ruffini corpuscles detect heat.
Pain is transmitted through naked nerve endings located in the basal layer of the epidermis.
Heat, cold, and proprioception also are located in the superficial dermis.
Cutaneous nerves follow the route of blood vessels to the skin. The area supplied by a single spinal nerve, or a single segment of the spinal cord, is termed a dermatome. Adjacent dermatomes may overlap considerably.
Read more about Dermatomes and Myotomes of Lower Limb
Nerve bundles, together with arterioles and venules, are found in a great quantity in neurovascular bundles of the dermis.
Vasoconstriction is regulated by the postganglionic adrenergic fibers of the autonomic nervous system. This regulates the apocrine gland secretions and the contraction of arrector pilli muscles of hair follicles.
Eccrine sweat secretions are mediated by cholinergic fibers.
Functions of Skin
Protection
The skin protects the underlying structures from:
- Ultraviolet radiation
- Dehydration minimizing the water loss
- Destruction of microorganisms & interaction of skin with the body’s immune system
- Langerhans cells (of the epidermis)
- Phagocytic cells
- Epidermal dendritic cells
- Mechanical trauma / physical injuries
Sensation
- Pressure/touch, heat/cold, pain
Temperature Regulation
Skin tissue causes retention or release of heat depending on the outside temperature for regulating body temperature. It is done by regulation of blood flow to the skin especially of the extremities.
This is achieved by the skin’s natural heat conductivity and loss of heat from the evaporation of sweat and convection from cutaneous vessels.
The thermoregulatory center in the hypothalamus controls vasoconstriction and vasodilatation of cutaneous vessels through the sympathetic nervous system.
Vasodilation and increased skin blood flow, along with sweating, are crucial to heat dissipation during heat exposure and exercise. During exposure to cold, vasoconstriction in the skin decreases heat loss from the body to prevent hypothermia.
Movement & Growth
Skin accommodates the growth of the body and bodily tissues and adapts the contours of the body during movement. It is achieved by elastic and recoil properties of the skin.
Lines and creases are evident over major and minor joints for this purpose.
Relaxed skin tension lines are created by the natural tension on the skin from underlying structures.
Excretion
Excretion of water, urea, ammonia and uric acid occurs, though not significantly, in the sweat.
Endocrine Function
Synthesis of Vitamin D occurs in the skin. Vitamin D is made when an organic chemical in the skin called 7-dehydrocholesterol reacts with UVB ultraviolet light.
Lipid Storage
The hypodermis has the adipose tissue present consisting of fat-storing cells called adipocytes. This stored fat can serve as an energy reserve.
Skin Pigmentation
The amount of melanin pigment in the skin determines an individual’s skin color. Skin pigment can be inherited genetically and is influenced by a number of pigments, including melanin, carotene, and hemoglobin.
Melanin is produced by cells called melanocytes, which are found scattered throughout the stratum basale of the epidermis. The melanin is transferred into the keratinocytes via a cellular vesicle called a melanosome.
Melanin occurs in two primary forms. Eumelanin exists as black and brown, whereas pheomelanin provides a red color. Dark-skinned individuals produce more melanin than those with pale skin.
Aging of Skin
Male skin is thicker than female skin in all anatomic locations. Children have relatively thin skin, which progressively thickens until the fourth or fifth decade of life when it begins to thin. Thinning is also primarily a dermal change, with loss of elastic fibers, epithelial appendages, and ground substance.
Aging features are skin laxity, fragility, and wrinkles. Sun-exposed areas also demonstrate dyspigmentation, premature wrinkling, telangiectasia, and actinic elastosis.
Sun exposure and smoking amplify skin aging due to the destruction of the cellular structure of the skin, and in severe cases, can cause sufficient DNA damage to result in skin cancer.
