Last Updated on October 28, 2023
Parenteral nutrition is the feeding of a person through intravenous route by providing nutritional formulae that contain nutrients.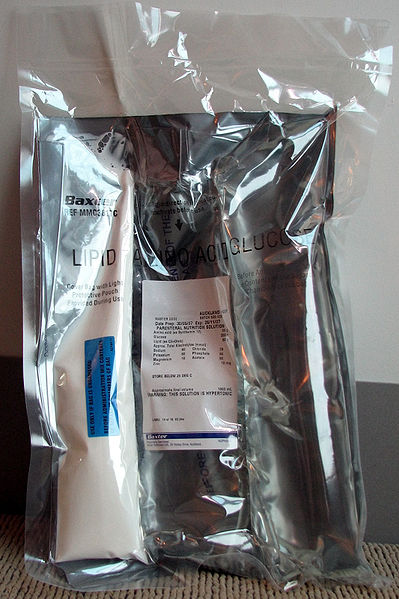
Parenteral nutrition could be total or partial. Total parenteral nutrition or total nutrient admixture is when no significant nutrition is obtained by other routes [entral].
Partial parenteral nutrition is used when nutrition is also partially enteric.
Depending on the access, the nutrition may be called peripheral parenteral nutrition when administered through vein access in a limb or central venous nutrition when administered through central vein.
Parenteral nutrition is used in less than 4—5 per cent of all hospital admissions.
It is used either when enteral feeding is not possible, or to supplement deficient enteral feeding.
Parenteral nutrition is not without the risks and is used in cases when the benefits outweighs the risks.
Displacement of the catheter, sepsis, mechanical problems and metabolic derangements are the common complications of the parenteral nutrition.
Indications
Parenteral nutrition is indicated for all patients who are either malnourished or at risk of malnutrition and cannot be fed entrally.
Enteral feeding is preferred over parenteral feeding in inpatients with functioning gastrointenstinal tracts.
Parenteral nutrition can be considered in following situations
- Gastrointestinal disorders
- Bowel obstruction
- Short bowel syndrome
- Gastroschisis,
- Prolonged diarrhea regardless of its cause
- High-output fistula
- Very severe Crohn’s disease
- Ulcerative colitis
- Congenital GI anomalies
- Necrotizing enterocolitis
- Perioperative nutritional support
- Patients with high risk of prolonged postoperative ileus
- Pancreatitis and pancreatic fistulae
- Palliative surgical and non-surgical oncology
Contraindications
- Cardiac failure
- Severe liver disease
- Disorders of fat metabolism
- Uncontrolled diabetes
- Shock
- Severe blood dyscrasias
- Inexperienced hands.
Parenteral Nutrition Feed preparations
Nutritional requirements are calculated for the patient depending on his/her requirement of carbohydrate, fat, protein, vitamins, minerals and trace.
Solution for total parenteral nutrition contain a balanced mix of essential and non-essential amino acids, glucose, fat, electrolytes and micronutrients:
Parenteral nutrition should be introduced at a low rate and gradually increased.
Parenteral nutrition can either be given at a continuous rate or in cyclical regimen.
Vitamins including folic acid are infused with the solution, but vitamin B12 must be prescribed separately.
Solutions for total parenteral nutrition may be customized to individual patient requirements, or standardized solutions may be used.
Monitoring
Patients on parenteral nutrition should be monitored. It involves observations and laboratory investigations.
Apart from vital sign monitoring and other clinical signs, the patient should be daily monitored for signs of inflammation or infection at the site for catheter. Signs of thrombophlebitis may be looked for.
Patient should be periodically investigated for. The frequency depends on the condition of the patient.
- Complete blood count daily
- Vitamin B12 levels
- Folate levels
- Magnesium, phosphate and calcium levels every 3 months
- Zinc, iron, selenium and copper levels – every 2-4 weeks.
- Blood glucose levels every 4-6 hours
- Liver function tests twice weekly
- Serum protein levels twice weekly
- Inflammatory markers – ESR and C-reactive protein
The frequency of most tests can be reduced once the patient’s condition is stable.
Complications
- Infection of catheter
- Most frequent
- Septic shock can occur
- Common cause of death
- Blood clots and pulmonary embolism
- Thrombolytic flush can help
- Fatty liver and liver failure
- Hungermpangs
- Failure of satiation as patient does not eat
- Hepatobiliary Dysfunction
- Cholecystitis
- Chlestasis
- Cholelithiasis
- Gut atrophy in infants
- Catheter complications
- Pneumothorax
- Accidental arterial puncture
- Catheter-related sepsis.
- Metabolic complications
- Hypokalemia- decrease in potassium levels
- Hypophosphatemia – decrease in phosphate levels
- Hypomagnesemia – decrease in magnesium levels
- Hyperglycemia -High levels of glucose
- Hypoglycaemia -Low levels of glucose
- Refeeding syndrome
- Starvation depletes intracellular phosphate.
- Feeding stimulates the cellular uptake.
- Results in electrolyte imbalance.
- Rhabdomyolysis, cardiac failure, hypotension, arrhythmias, respiratory failure, seizures and coma can occur.
Home Nutrition
Chronic intestinal failure results in a failure of adequate nutrient absorption from the gut to maintain body weight. This may follow extensive bowel resection, multiple high output fistulas, motility disorders and extensive Crohn’s disease. Such patients require prolonged nutritional supplementation at home parenteral nutrition.
Patients must receive training and information on nutrition prior to discharge.
Patient should be confident in the management of feeding systems and aware of common issues.
There must be a fall back option where patient can ask for help.
