Last Updated on October 28, 2023
The Pap test or the Pap smear is a screening test to detect cervical cancer.
In Pap testing, cells are collected from the cervix which is the lower end of the uterus. These cells are then examined microscopically to look for any abnormality. The significance of this procedure lies in the fact that it can detect both cancerous as well as precancerous cells present in the cervix. Presence or suspicion of precancerous/ abnormal cells can be confirmed by other advanced diagnostic techniques.
The test was invented by George Papanicolaou, who was a Greek pioneer in cytopathology and is named after him.
While the test may also detect infections and abnormalities in the endometrium, its primary utility remains to detect cervical lesions.
Who needs a Pap smear? When to Have a Pap Smear
Screening guidelines vary from country to country. It is recommended that pap test screening be carried out every 3 years starting from the age of 21 years till 65 years.
Screening is not required in women less than 21 years old even if they are sexually active because the incidence of cervical cancer in this age group is extremely low and precancerous lesions usually clear on their own.
After 30 years, the test may be carried out every 5 years provided that HPV testing is done simultaneously and the previous pap tests have all been negative.
Women after the age of 65 years and having a history of normal pap test results do not require any further testing. Also there is no need to continue screening after a complete hysterectomy for benign disease.
Women having increased risk of cancer (HIV positive or those having weakened immune status) may need more frequent testing. Women who are virgins i.e., those who have never had vaginal intercourse are at an extremely low risk for cervical cancer, but may consider pap testing.
If any abnormality is detected, the test may have to be repeated in 6 to 12 months. In case of some severe abnormality, it may be necessary to carry out further investigations including colposcopic visualisation of cervix and biopsy.
Pap smear screening is still recommended for those who have been vaccinated against HPV since the vaccines do not cover all of the HPV types that can cause cervical cancer. Also, the vaccines do not provide protection if the patient has been exposed to HPV exposure before vaccination.
Pap tests can be performed safely during pregnancy up to at least 24 weeks. Pap tests during pregnancy have not been associated with increased risk of miscarriage. After childbirth, pap test should not be done before 12 weeks because inflammation of the cervix caused by the birth interferes with test interpretation.
Effectiveness of Pap Smear
Cervical cancer is one of the most common cancers prevalent world-wide. In the developing world, it remains the most common cause of cancer death. About 70% of cervical cancers occur in the developing world. The widespread awareness and use of cervical screening programs in developed world has led to a marked reduction in the incidence of advanced cervical cancers. Pap test along with an appropriate follow-up has been shown to reduce deaths due to cervical cancer by up to 80%.
Results of Pap Smear
Pap smear is reported according to the Bethesda system.
[Read more about Bethesda system of reporting Pap]
When a general or low-risk population is screened, most Pap results are normal.
Abnormal squamous cells of undetermined significance or ASC-US
It constitutes 2–5% of Pap results.
Low-grade Squamous Intraepithelial Lesion or LSIL
is found in approximately 2% of patients. Although most low-grade cervical lesions regress spontaneously and do not lead to cervical cancer, they usually indicate an increased need of monitoring and follow-up.
High-grade Squamous Intraepithelial Lesion or HSIL
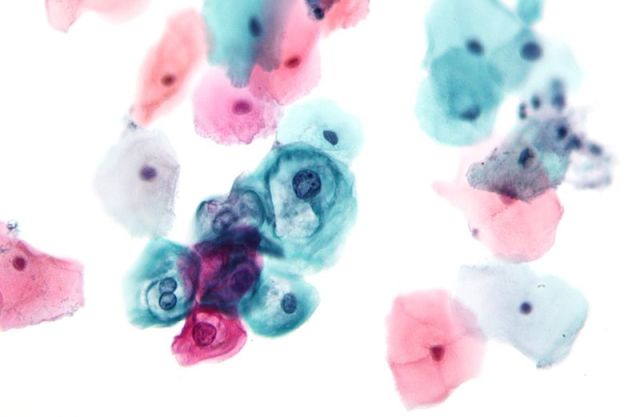
About 0.5% of Pap results are high-grade SIL (HSIL), while invasive cervical cancer is seen in 0.5% of results. Atypical Glandular Cells of Undetermined Significance (AGC-NOS) is found in < 1% of results.
When Pap Smear Should not Be Done?
Ideally, the Pap test should not be done during the menstrual phase because blood and endometrial cells can obscure the cervical cells leading to problems in interpretation. Sexual intercourse, douching or use of spermicidal agents should be avoided for 2 days before the test.
Is Pap Smear Painful?
If carried out gently, the pap test procedure does not cause significant pain although it might cause some discomfort. In patients having cervical stenosis or vaginismus, the test might be painful. Using wrong sized speculum can also result in greater discomfort. Warming the speculum and use of lubricants can significantly reduce patient’s discomfort.
Some women experience spotting or mild diarrhea after the procedure. Spotting occurs due to the trauma inflicted on the cervix during scraping of cells while diarrhea is the result of indirect stimulation of the lower intestine during the procedure.
Procedure of Pap Test
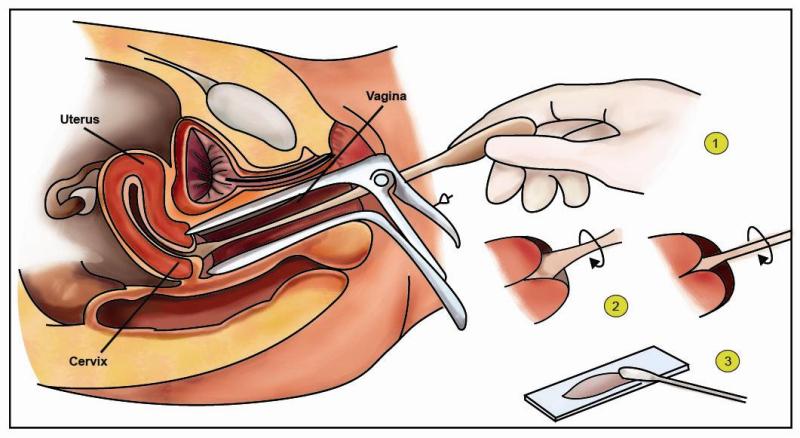
- The patient is asked to lie on her back on an examination table with the legs spread and the feet resting in supports called stirrups.
- An appropriately sized speculum is inserted into the vagina (warm water may be used to lubricate the speculum if necessary). This opens and spreads the vagina, thereby making the cervix visible. Any excessive discharge or mucous present on the cervix is gently wiped away with a sterile swab.
- A sample of cells is scraped from the outer opening or os of the cervix using a spatula. An endocervical brush is then inserted into the endocervical canal and gently rotated to collect cells from the cervical canal.
- A cytobrush which is a combination of spatula and brush; or a plastic-fronded broom can also be used.
- For conventional testing: Both the spatula and brush are smeared on a glass slide. The slide is immediately fixed by either immersing it in a jar containing appropriate fixative or spraying of the fixative on to the slide.
- For liquid based cytology: The spatula and brush are immersed in the liquid vial and rinsed or swirled vigorously to release the contents in the vial.
- The fixed slide or the liquid vial is then transported to the lab.
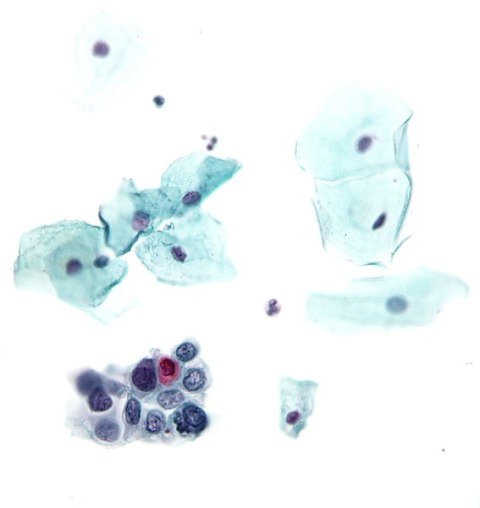
- After fixation, the slide is stained using the Papanicolaou technique, in which tinctorial dyes and acids are selectively retained by cells.
- The slide is sent to pathologist for reporting
Automated analysis
In recent years, automated, computer image analysis systems have been developed for screening of pap smears. Automation improves sensitivity and reduces the number of unsatisfactory specimens.
The computer system screens the slides, segregating those cases which do not need further manual screening. Cases which require further examination are then screened by specially trained and qualified personnel – cytotechnologist or pathologists using a light microscope. The automated system also highlights the areas containing suspicious cells which can be thoroughly examined manually.
SurePath and ThinPrep 2000 System are two such systems.
With both methods, the sample is collected as in liquid-based cytology (LBC). Liquid-based cytology has manifold advantages over the conventional testing.
In the conventional method, not all the cells that are scraped off get transferred to the slide. Liquid-based cytology, however, ensures that all the representative material is transferred to the slide. Liquid-based cytology keeps the cells well-preserved and present in a monolayer resulting in greater accuracy of results.
These slides, being cleaner and devoid of background blood make the interpretation easy.
Moreover, screening of normal cases with automated system markedly reduces the manual work load.
Additional molecular and biomarker tests can be carried out with LBC and not with conventional smears.
The only disadvantage of LBC is the high cost involved.
Limitations of Pap smear cytology
- There is a low sensitivity for detecting pre-cancerous lesions.
- ASC-US cytology is not specific for pre-cancerous lesions. It also includes many reactive conditions attributable to infections.
- Pap testing has a low sensitivity for detecting glandular cell abnormalities including adenocarcinoma.
- There is a highly variability in results between different laboratories.
- Failure to sample the suspicious area can lead to a false negative result.
- It requires women to be screened at frequent intervals.
Human Papilloma Virus Co-testing in Pap Smear
Sexually acquired infection with certain types of HPV (Human papillomavirus) is a major cause of cervical cancer. Therefore HPV co-testing is advised.
There are more than 100 types of HPV, of which at least 13 are cancer-causing (also known as high-risk type). Two HPV types (16 and 18) cause 70% of cervical cancers and precancerous cervical lesions.
It is recommended that HPV testing be done simultaneously along with the pap test. This reduces the chances of missing an abnormality ie, reduces false negative results. It includes high-risk HPV testing and HPV 16 and HPV 18 genotyping.
A woman who has a normal Pap result and a negative HPV test have a very little chance of a serious abnormality developing in near future. Also, in such patients, screening can safely be done at an interval of 5 years.
HPV co-testing also increases the detection of glandular cell abnormalities, including adenocarcinoma of the cervix. Pap testing has a much lower sensitivity to detect glandular cell abnormalities in comparison to much more prevalent squamous cell abnormalities.
Follow up of Abnormal pap result
Any abnormal pap result requires a follow-up with the doctor.
Most women with abnormal result of ASC-US [Atypical squamous cells of undetermined significance] do not need special treatment. All they need is regular or more frequent pap testing to detect significant cellular changes. Most of the times, ASC-US changes are due to an underlying treatable cervical or vaginal infection or due to low risk type HPV infection which will clear itself within a few months.
Wait and watch policy is justified in low grade abnormalities including ASC-US and LSIL [low grade squamous intraepeithelial lesion] as they will either go away on their own or are unlikely to become more severe in a short period of time.
Further testing
The doctor may ask for the following tests to be carried out in case of abnormal pap result. These include
- Tests for infections: including sexually transmitted infections, candidiasis and bacterial infection.
- HPV testing – This is done to detect the type of HPV infection. Presence of high-risk types of HPV indicates greater propensity for more severe lesions in future.
- Colposcopic evaluation of cervix – In this test, the doctor uses a magnifying instrument to look at vagina and cervix. If any suspicious area is observed, a cervical biopsy (a small sample of tissue) can be taken for microscopic evaluation.
- Cone biopsy . Major abnormalities including HSIL [high grade squamous intraepeithelial lesion] usually require a cone biopsy. In this, little more tissue is removed than a cervical biopsy. In some cases, it also serves as treatment by removing the abnormal cells.
Treatment of Abnormal Pap Result
Treatment depends on the underlying cause.
- Any fungal or bacterial infection has to be treated accordingly.
- A pregnant woman with an abnormal Pap test is monitored closely throughout her pregnancy. Monitoring may include a colposcopy. The goal is to rule out cervical cancer, a rare diagnosis. If cancer is ruled out, treatment for abnormal cell changes is done after delivery.
- Women in perimenopausal or menopausal age may show abnormal results due to the atrophic changes usually seen in this age group. These changes will clear up with the local use of estrogen creams.
- Treatment of HSIL includes destroying or removing the abnormal tissue. Treatment choices include –
- Cone biopsy.
- Loop electrosurgical excision procedure (LEEP), which uses a thin, low-voltage electrified wire loop to cut out abnormal cervical cells.
- Cryotherapy, which destroys abnormal cervical cells by freezing them.
- Laser therapy, which uses a laser beam to destroy abnormal cervical cells.
- Treatment of cervical cancer depends on the stage of cancer and includes surgery, radiotherapy and chemotherapy.
