Last Updated on January 12, 2020
Mastitis is an inflammation of the breast due to an underlying infection. It causes the breasts to become swollen and painful. Although it can occur in any woman, it most commonly occurs in women who are breastfeeding.
It is important to treat mastitis early to prevent complications. The mother should continue breastfeeding as it helps to drain the milk and promotes healing of the condition.
In this article, we shall discuss the causes, signs and symptoms, measures to prevent as well as treatment of mastitis.
What Is Mastitis?
Mastitis occurs due to inflammation of the breast tissue usually due to an underlying infection.
It most commonly affects breastfeeding mothers in the first 3 months of childbirth. It is also referred to as lactation mastitis or puerperal mastitis.
However, it can occur even during the later period of breastfeeding or sometimes in non-breastfeeding women as well.
In non-breastfeeding women, mastitis most often occurs when the breast becomes infected as a result of damage to the nipple, such as a cracked or sore nipple, or a nipple piercing. It is also called periductal mastitis.
Due to the pain that occurs in mastitis, many mothers are tempted to wean their babies. However, it is advisable to continue breastfeeding during mastitis even while taking an antibiotic. Breastfeeding actually helps to prevent and relieve mastitis. Needless to say, breast milk provides numerous health and psychological benefits to both the mother and the baby.
Read more about Breastfeeding – Benefits, Problems, and Tips for Better Feeding
Signs and Symptoms of Mastitis
- Pain or burning sensation in the breast either continuously or during breastfeeding
- Tenderness or soreness of the breast
- Swelling of the breast
- Feeling of warmth in the breast
- Redness of the skin of the breast
- Vague thickening of breast tissue, or presence of a breast lump
- Feeling ill and tired
- Fever and chills
- Nipple discharge, which may be white or streaked with blood
Causes of Mastitis
For the initial 2 to 3 days after delivery, the breasts produce a thick and yellowish fluid called colostrum. After these few days, the quantity of milk produced by the breasts increases. The breast tissue gets filled with milk, blood, and other fluids causing the breasts to feel hard and painful. This condition is called breast engorgement.
Read more about Breast Engorgement: Causes, Prevention, and Treatment
Breast engorgement is a normal phenomenon that occurs due to hormonal changes and increased milk production.
Read more about Breast Milk Production and Regulation
Despite being painful, breast engorgement is a temporary problem and usually resolves on its own within 1 or 2 days. In some cases, however, it does not resolve on its own and the breast tissue may get infected resulting in mastitis.
This occurs due to the following reasons:
- Incomplete emptying of the breast: If the breast does not empty fully, the trapped breast milk can lead to infection of the breast tissue. Incomplete emptying can be due to
- Improper latching of the baby to the breast.
- The mother is producing more milk than what the baby is able to consume or the breasts can hold.
- Giving formula feed to the baby in addition to breast milk resulting in lesser intake of breast milk by the baby.
- Missing several feeds because of separation from the baby due to work or other factors.
- Blocked milk duct: If a breast is not completely emptied after feeding, one of the milk ducts can become clogged. This can cause a build-up of milk, ultimately leading to breast infection.
- Cracked or sore nipples: Bacteria present on the mother’s skin or the baby’s mouth can enter the breast tissue through a break or crack in the skin of the nipple. Breast milk acts as a breeding ground for bacteria resulting in mastitis.
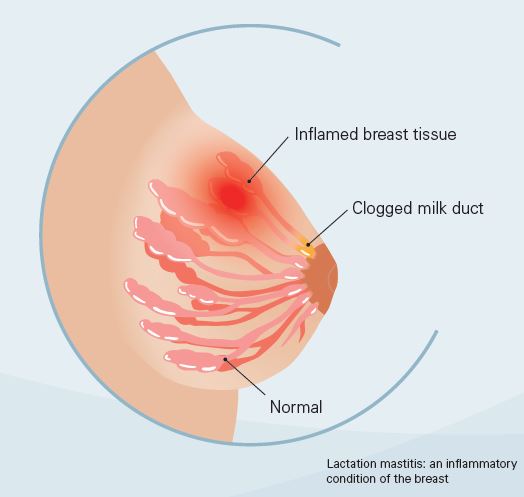
Image credit: https://www.nestlenutrition-institute.org
In non-breastfeeding women, mastitis occurs when the breast becomes infected either due to damage to the nipple (a cracked or sore nipple) or in cases of nipple piercing.
Mastitis can also occur in non-breastfeeding women due to duct ectasia. It occurs when a milk duct under the nipple widens. The wall of the duct gets thickened and the duct is filled with a thick, sticky substance that may get infected.
Women suffering from diabetes, chronic illness, AIDS, or having reduced immunity may also develop mastitis.
Risk Factors for Mastitis
- Extreme stress or tiredness
- Poor nutrition
- A previous episode of mastitis
- Wearing a tight-fitting bra which can restrict milk flow by putting pressure on the breast.
How to Prevent Mastitis?
During the initial days of breastfeeding
The key to prevent mastitis is to prevent engorgement so that milk does not remain accumulated within the breast.
- Ensure proper latching of the baby to the breast. It is very important to learn the proper technique of breastfeeding so that each breast is fully emptied after feeds.
- Try to feed the baby in different breastfeeding positions. This may help the baby latch on properly and feed more effectively.
- Feed the baby often and on-demand (not by the clock). At least 8 to 12 feeds should be given every day (including night time) especially in the initial days.
- Avoid giving the baby any fluids other than breast milk unless there is a specific medical reason. No water or formula milk should be given as they will reduce the baby’s thirst, hunger, and need for breast milk.
- Do not wear a tight-fitting bra as it prevents the proper flow of milk.
- If due to any reason, the mother has to miss a feed, she should express the milk either manually or with the help of a breast pump.
Read more about Breast Pump: Types, Working, Uses and Selection tips
During later stages of breastfeeding
Weaning the baby from breastfeeding should be carried out gradually. Do not stop at once as it may lead to a large quantity of retained milk in the breast which can lead to mastitis.
Should a Mother Continue Breastfeeding during Mastitis?
Yes, a mother can breastfeed during mastitis. Breast milk does not get contaminated during mastitis and is safe for the baby. The antibacterial properties of breast milk actually help protect the baby from the infection. (However, in case of breast abscess, breastfeeding from the affected side should be avoided.)
Because of the pain that occurs during breastfeeding, it is natural for a mother to think about weaning her baby during mastitis. But it is very important for the mother to continue breastfeeding from the affected side as well, as it helps to resolve the condition faster by draining the breast.
The mother should consult her doctor who can treat her mastitis by prescribing antibiotics that are safe for the baby (since they will enter the breast milk).
Complications of Mastitis
Breast abscess
If not treated in time, mastitis can worsen and result in the formation of a breast abscess filled with pus. Once an abscess is formed, it needs to be surgically incised and drained. Therefore it is important to recognize mastitis in the initial stages and treat it appropriately.
Chronic mastitis
Incomplete drainage of the breast abscess can result in chronic infection. It is usually seen in postmenopausal women and is associated with chronic inflammation of the ducts below the nipple. Hormonal changes in the body can result in the milk ducts becoming clogged with dead skin cells and debris. This results in the breast becoming more susceptible to bacterial infection.
Diagnosis
The diagnosis of mastitis can usually be made based on the signs and symptoms along with a physical examination of the breast.
To confirm the diagnosis, the following investigations may be carried out.
Ultrasound
It is a non-invasive investigation in which an ultrasound probe is placed over the affected area of the breast. It can help to distinguish between mastitis and a solid breast mass due to tumors. It can also help to differentiate between mastitis and a breast abscess.
Fine needle aspiration cytology (FNAC)
In this procedure, a fine needle is inserted into the lump or affected area and some material is aspirated which is then examined under a microscope. It is a quick, relatively painless, non-invasive, outdoor procedure. It can help to confirm the infective nature of the disease.
Culture and sensitivity
Small material aspirated during FNAC may be sent for culture techniques. It helps to identify the organism responsible for the infection. In addition, it also gives information about the most suitable antibiotic which will be effective against that organism.
Mammography and Biopsy
Mastitis in nonbreastfeeding women or which is not responding to treatment or is recurring should be investigated further. This is because a rare form of breast cancer (inflammatory breast cancer) can have redness, swelling and other symptoms similar to mastitis. Mammography and biopsy can help to rule out cancer.
Read more about Breast Cancer: Risk Factors, Classification, Diagnosis and Treatment
Read more about Inflammatory Breast Cancer : Clinical Features, Diagnosis and Treatment
Self-Care Tips for Mastitis
- Continue breast-feeding. Do not miss feeds or abruptly stop feeding as it will worsen the engorgement.
- If breastfeeding is too painful, try to pump breast milk or express it by hand.
- Provide adequate support to breasts by wearing a properly fitting bra.
- Drain the breasts regularly and completely during breast-feeding.
- If after a feed, the breasts still feel firm, express more milk either manually or by breast pump till the breasts feel softer.
- Take a warm shower or apply a warm wet sterile piece of cloth on to the breast. This will help to relieve pain and promote the easy flow of milk.
- Ensure proper latching of the baby to the breast. For learning proper technique, consult a lactation consultant or breastfeeding specialist.
- A different breastfeeding position can be tried so that minimum pressure is exerted on to the painful area of the breast.
- Keep the breasts and nipples clean. Lukewarm water can be used to remove any dried milk or debris present on the nipples which may be blocking the flow of milk.
- Express a small amount of milk before feeding by gently squeezing the breast. This makes the breasts and nipple soft and promotes easy flow of milk.
- Gently massage the breasts in a downward motion from the chest wall till the nipple during feeding so that milk comes out easily.
- Remain well hydrated and eat a well-nourished and balanced diet.
Treatment for Mastitis
Antibiotics
A complete course of oral antibiotics should be taken to completely eradicate the infection. Do not stop taking the medicine as soon as the symptoms or fever subside.
Pain relievers
An over-the-counter pain reliever or analgesic, such as acetaminophen or ibuprofen may be taken to relieve pain, inflammation, and fever.
Incision and drainage
If an abscess develops, pus needs to be drained after giving a surgical incision. In addition, IV antibiotics may have to be administered.
Prognosis or Long Term Outlook
If treated adequately and well in time, mastitis heals completely without any serious short-term or long-term complications. The majority of the women can and should continue breastfeeding from both the breasts even if they have mastitis.
Mastitis does not cause cancer. However, a rare form of breast cancer can mimic mastitis. Hence it is important to rule out cancer if the patient is not responding to treatment.
