Last Updated on August 29, 2023
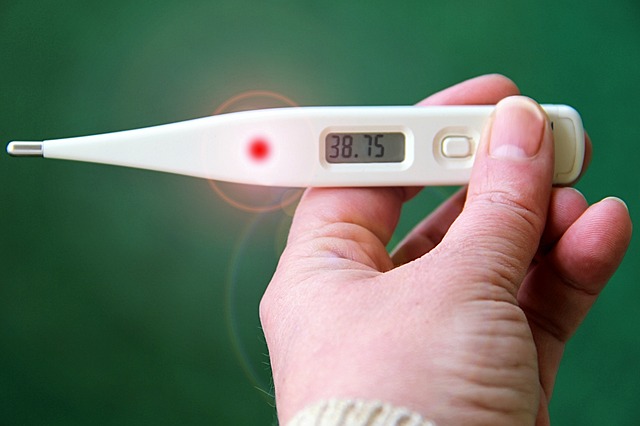
Normal body temperature changes in response to many conditions. fever is nothing but an increase in body temperature due to the release of pyrogens in response to external stimuli. Therefore, it often becomes necessary to measure body temperature to find and document abnormal temperatures. There are many methods to measure body temperature.
Normal Body Temperature and Its Variations
Human body temperature is measured in Fahrenheit or Celsius. It is a common belief that normal human body temperature is 98.4 degrees Fahrenheit or 37 degrees Celsius.
But what most people think of as a “normal” body temperature is an average of normal body temperatures in a large population of people. An individual person’s temperature may actually be 1 °F (0.6°C) or more above or below 98.6 °F.
Moreover, the body temperature may vary with time of the day. Your normal body temperature changes by as much as 1°F (0.6°C) throughout the day, depending on how active you are and the time of day. Body temperature is very sensitive to hormone levels and may be higher or lower when a woman is ovulating or having her menstrual period.
How to Measure Body Temperature by Different Methods?
Oral Method
This is the most common method of taking body temperature.

The person should be mature enough to cooperate and follow instructions. He should not have taken any hot or cold stuff for some time.
For accurate measurement, it is important that the person whose temperature is to be taken should be able to breathe through the nose.
If the nose is stuffy or the patient does not cooperate, the reading will be faulty. In such cases, it is always better to use other methods.
- The person is asked to place the thermometer under the tongue, on one side of the center. The lips should be tightly closed around it.
- Leave the thermometer in place for the required amount of time. The time period varies from thermometer to thermometer. Traditionally, the mercury thermometers were kept for three minutes. Keep the thermometer for the required time. Digital thermometers give beeps on completion of reading.
- Check the reading on the thermometer after taking it out from the mouth after the required time.
- Clean the thermometer with clean water.
Rectal Method
- This method is recommended for infants, small children, and people who are unable to hold a thermometer safely in their mouths. Rectal temperature gives the most accurate measurement of body temperature.
- Apply a lubricant on the bulb of the thermometer. A jelly-like Vaseline would do. This makes the insertion of the thermometer easier.
- In the case of children, make the child lie prone on a lap or soft padded surface.
- Spread the buttocks and insert the bulb end of the thermometer about 1/2 to 1 inch into the anal canal. Be careful not to insert the thermometer too far. Prevent the child from struggling, since this can accidentally push the thermometer in further. Remove the thermometer after 3 minutes or when the device beeps. Pressing the child’s buttocks together will help keep the thermometer in place.
- Remove the thermometer and read it. A rectal temperature reading may be as much as 1°F (0.6°C) higher than an oral temperature reading.
- Clean the thermometer with cool, soapy water and rinse it.
A thermometer used for measuring rectal temperature should not be used to measure oral temperature.
Armpit Method

Though not as accurate as oral or rectal methods, the armpit is commonly used as a place for measuring the temperature. It is quite a simple method to execute.
- The thermometer is placed underarm with the bulb in the center of the armpit.
- Press the arm against the body. The usual time for which the thermometer is kept is 5 minutes.
- Remove the thermometer and read it. An armpit temperature reading may be as much as 1°F (0.6°C) lower than an oral temperature reading.
- Clean the thermometer with cool, soapy water and rinse it off before putting it away.
From Ear
For this measurement, one requires special thermometers.

- Check that the probe is clean and free of debris. If dirty, wipe it gently with a clean cloth. Do not immerse the thermometer in water.
- Attach the disposable cover to the probe. Use a disposable probe cover to keep the probe clean. Use a new probe cover each time you take an ear temperature.
- Turn the thermometer on.
- For children < 12 months, pull the earlobe down and back to place the probe in the ear canal. Center the probe tip in the ear and push gently inward toward the eardrum.
- For children >12 months and adults, pull the earlobe up and back.
- Press the “on” button to display the temperature reading.
- Remove the thermometer and throw away the used probe.
Remote [non-contact] thermometers can also be used for measuring temperature from the ear.
Forehead
Again, specialized devices are required for this measurement. You must have come across the forehead temperature scanners during COVID at the airport theaters etc. The following site was common in those times.
This type of thermometer is a non-contact or remote thermometer. Another type is a contact thermometer that uses a cup to be placed against the forehead.
Using a Contact Thermometer on the Forehead
- Press the soft cup of the thermometer or the entire plastic strip firmly against a dry forehead.
- Hold the thermometer in place for the required time.
- Read the temperature before removing the thermometer. [Note the difference from other methods]
- Clean the thermometer.
Remote thermometers are aimed at the forehead from a distance. They use infrared scanners to know the temporal artery temperature.
Using a no-touch forehead thermometer
 Power on and let the device be ready
Power on and let the device be ready- Position the thermometer about 5 cm from the center of the forehead. A light on some devices might help you to position
- The device beeps in 2-3 seconds when it is ready for the reading
Forehead thermometers are not as accurate as other thermometers. In case of high fever, the temperature should be confirmed by other methods.
References
- Mogensen CB, Wittenhoff L, Fruerhøj G, Hansen S. Forehead or ear temperature measurement cannot replace rectal measurements, except for screening purposes. BMC Pediatr. 2018 Jan 26;18(1):15. doi: 10.1186/s12887-018-0994-1. [Link]
- Niven DJ, Gaudet JE, Laupland KB, Mrklas KJ, Roberts DJ, Stelfox HT. Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med. 2015;163(10):768–777. doi: 10.7326/M15-1150. [Link]
- Batra P, Goyal S. Comparison of rectal, axillary, tympanic, and temporal artery thermometry in the pediatric emergency room. Pediatr Emerg Care. 2013;29(1):63–66. doi: 10.1097/PEC.0b013e31827b5427. [Link]
